Surgical Techniques for HS 2: Mini-Unroofing and Deroofing
Warning – this post contains graphic content / imagery.
Introduction:
We previously introduced some of the common techniques used for the surgical treatment of HS, summarised in this excellent short (~ 1 min) informational video from WebMD. Much of the information in these posts examining HS surgical techniques is summarised in the open-access review by Scuderi et al. (2017). Other comprehensive HS surgery reviews include Danby et al. (2015) and Janse et al. (2016).
Mini-Unroofing and Deroofing: An Overview
First described over half a century ago (in 1959), one surgical strategy that has grown enormously in popularity in more recent years for treating HS is deroofing (also referred to as unroofing in the literature). Although there are some variations of the technique, (outlined below), the basic principal of each is more or less the same, illustrated here:
In deroofing, the top or “roof” of the HS lesion is surgically removed (partially in mini-unroofing or completely in deroofing) and the wound is left to heal from the bottom up (known as secondary intention healing). We will now look at the main deroofing techniques in more detail.
Punch Debridement/Mini-Unroofing:
In a previous post, we examined the popular surgical technique known as incision and drainage (I & D), a well-established strategy that is very effective at relieving pain in acute HS flares and well-suited to stage I HS in the Hurley classification system. Another strategy growing in popularity for the treatment of acute flares in stage I HS is mini-unroofing or punch debridement, illustrated in the WebMD HS surgery video from ~ 29 to 41 seconds.
In punch debridement/mini-unroofing, after applying local anaesthetic to the affected area, a tool known as a punch biopsy is used to extract the top 5–8 mm of skin of the HS lesion, and the wound is then left to heal. Here is a ‘before and after’ series of images of the area under a female breast affected by HS that has had punch debridement:

Punch debridement is well suited for acute stage I HS. It is relatively inexpensive, can be performed in just a few minutes in an office, surgery, or hospital accident and emergency department setting. In addition, it preserves the maximum amount of surrounding healthy tissue, and doctors and patients report the resulting surgical scars are generally cosmetically acceptable.
However, like I & D, mini-unroofing is not effective in treating chronic HS. In such instances, other surgical approaches are needed, and deroofing is one such technique.
Deroofing:
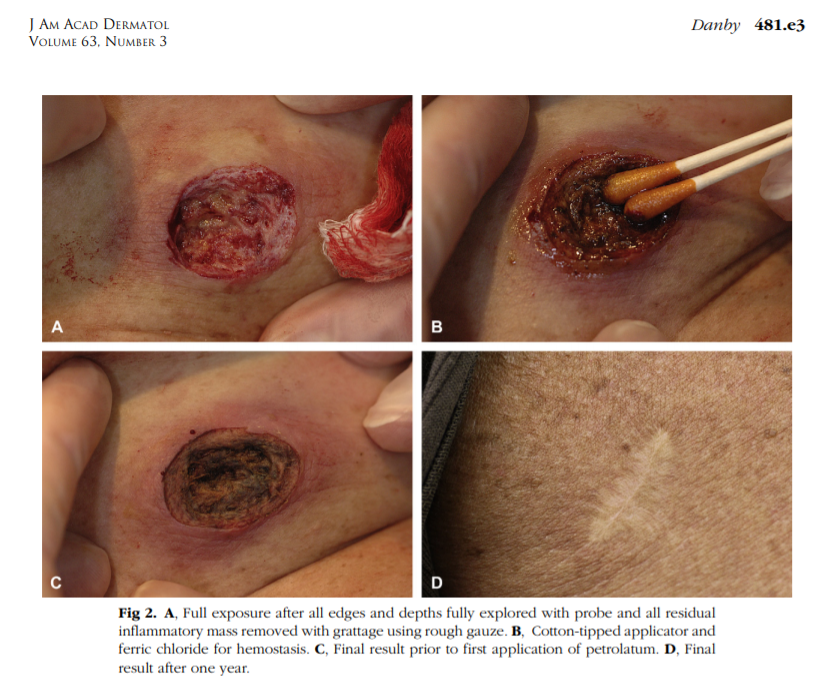
Like mini-unroofing, deroofing is a relatively inexpensive and fast procedure that is well suited to the office or surgery setting. In addition, deroofing also preserves the maximum amount of surrounding healthy tissue and the scars are usually acceptable to the patient. In this technique, usually performed by a dermatologist, a local anaesthetic is applied to the affected area(s) and the dermatologist uses a scissors, scalpel, electrosurgery, or a CO2 laser to remove the roof of the lesion. It can be used on a single lesion (local deroofing), or it may be used on all lesions in an affected body area (extensive deroofing).
The videos on this page illustrate the HS deroofing procedure, highlighting just how quick it can be:
https://www.cardiff.ac.uk/centre-for-trials-research/research/studies-and-trials/view/theseus
Many practising deroofing in their clinics report that the surgical scars resulting from deroofing are generally acceptable to patients.
- Groin HS treated with deroofing, before and 1 year after deroofing:

- Similarly, the surgical scar 1 year after this deroofing procedure is hardly noticeable:
Over the past decade or so, deroofing has been widely used to successfully treat stage I–II HS. Several long-term follow-up studies report that recurrence rates in deroofing are much improved over I & D procedures (which approach 100%) and comparable (from ~ 4% to < 30%) to more invasive excision surgery (reviewed in Janse et al., 2016 and in Kohorst et al., 2016; Scuderi et al., 2017). The only reported complication with deroofing reported so far is bleeding after surgery in a small number of cases (~ 1%). Janse et al. (2016) report a high satisfaction rate among HS patients, with ~90% reporting that they would recommend deroofing to other patients.
Expert opinion in the European (Zouboulis et al., 2015), North American (Alikhan et al., 2019), and Brazilian (Magalhães et al., 2019) guidelines for the treatment and management of HS all recommend deroofing (European: for stage I and II areas; North American: for acute and chronic wounds; Brazilian: in acute phases). In contrast, I & D is recommended in the North American and Brazilian guidelines only for acute HS abscesses to relieve pain, and not recommended at all in the European guidelines.
Despite the many advantages the technique offers, deroofing is limited in that it is usually effective only in stage I–II HS. More advanced HS (stage III) usually requires more complex surgery (excision).
Conclusions:
Due to the relatively low cost, rapid procedure times, minimum inconvenience for the patient, and overall effectiveness, the mini-unroofing and deroofing surgical techniques have been widely used in recent years for the treatment and management of HS. Many HS experts in the Americas and Europe are using these procedures in their clinics and are reporting promising results in the long-term management of HS. Patient-reported satisfaction with the procedures and outcomes are very high.
References:
Alikhan, A., Sayed, C., Alavi, A., Alhusayen, R., Brassard, A., Burkhart, C., Crowell, K., Eisen, D.B., Gottlieb, A.B., Hamzavi, I., Hazen, P.G., Jaleel, T., Kimball, A.B., Kirby, J., Lowes, M.A., Micheletti, R., Miller, A., Naik, H.B., Orgill, D. and Poulin, Y. (2019) ‘North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations: Part I: Diagnosis, evaluation, and the use of complementary and procedural management,’ J. Am. Acad. Dermatol., 81(1), 76–90, [online], available at: doi: 10.1016/j.jaad.2019.02.067, [accessed 27 Jul 2019].
Danby, F.W., Hazen, P.G. and Boer, J. (2015) ‘New and traditional surgical approaches to hidradenitis suppurativa,’ J. Am. Acad. Dermatol., 73(5 Suppl 1), S62–65, [online], available at: doi: 10.1016/j.jaad.2015.07.043, [accessed 27 Jul 2019].
Janse, I., Bieniek, A., Horváth, B., Matusiak, Ł. (2016) ‘Surgical procedures in hidradenitis suppurativa,’ Dermatol. Clin., 34(1), 97–109, [online], available at: doi: 10.1016/j.det.2015.08.007, [accessed 27 Jul 2019].
Kohorst, J.J., Baum, C.L., Otley, C.C., Roenigk, R.K., Schenck, L.A., Pemberton, J.H., Dozois, E.J., Tran, N.V., Senchenkov, A. and Davis, M.D. (2016) ‘Surgical management of hidradenitis suppurativa: outcomes of 590 consecutive patients,’ Dermatol. Surg., 42(9), 1030–1040 [online], available at: doi: 10.1097/DSS.0000000000000806, [accessed 27 Jul 2019].
Magalhães, R.F., Rivitti-Machado, M.C., Duarte, G.V., Suoto, R., Nunes, D.H., Chaves, M.H., Hirata, S.H. and Ramos, A.M.C. (2019) ‘Consensus on the treatment of hidradenitis suppurativa – Brazilian Society of Dermatology’, An. Bras. Dermatol., 94, (2 Suppl 1):7–19, [online], available at: doi: 10.1590/abd1806-4841.20198607, [accessed 27 Jul 2019].
Scuderi, N, Monfrecola, A., Dessy, L.A., Fabbrocini, G., Megna, M.and Monfrecola, G. (2017) ‘Medical and surgical treatment of hidradenitis suppurativa: a review’, Skin Appendage Disord., 3(2), 95–110, [online], available at: doi: 10.1159/000462979, [accessed 27 Jul 2019].
Zouboulis, C.C., Desai, N., Emtestam, L., Hunger, R.E., Ioannides, D., Juhász, I., Lapins, J., Matusiak Ł, Prens, E.P., Revuz, J., Schneider-Burrus, S., Szepietowski, J.C., van der Zee H,H. and Jemec, G.B. (2015) ‘European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa,’ J. Eur. Acad. Dermatol. Venereol., 29(4), 619–644, [online], available at: doi: 10.1111/jdv.12966, [accessed 27 Jul 2019].


